Guide to Applying a Vacuum or a Vacuum and Gas Flush to a Pouch

Your Step-by-Step Guide to Applying a Vacuum or a Vacuum and Gas Flush to a Pouch
Many manufacturers have questions about applying a vacuum only or a vacuum and gas flush to a pouch. In this blog post, we’ll explain:
- The most common applications for applying a vacuum or a vacuum and gas flush to a pouch
- How pouch materials impact which application is optimal and the best methods for working with common pouch material combinations
- The process for using a nozzle to apply a vacuum or a vacuum and gas flush to a pouch
- The process for using a chamber to apply a vacuum or a vacuum and gas flush to a pouch
Understanding these fundamental concepts and best practices will help you determine which application is optimal for your use case.
How to apply a vacuum or a vacuum and gas flush to a pouch
A vacuum or a vacuum and gas flush can be applied to a pouch in one of two ways—either by using a nozzle sealer or by placing the pouch in a chamber sealer. The optimal method is dependent on the type of pouch materials being used, whether vacuum only or vacuum and gas flush is required, and other factors.
A nozzle sealer is most commonly used for:
- Volume reduction. The goal of volume reduction is to remove enough air from the pouch to prevent it from popping during high altitude shipments or so that it can fit into a box or secondary container. Because volume reduction applications are considered a “gross” vacuum process, either time-based or level-based programs can be used; however, a time-based mode is the most popular. Product sensitivity can play a role in how much volume should be drawn out of the pouch.
- Product immobilization. In certain cases, it is critical to remove air from the pouch so that the product being packaged is immobilized. Product immobilization applications are considered a “gross” vacuum process so either time-based or level-based programs can be used; however, since the final internal volume in the pouch is a function for immobilizing the product, operating in level mode provides greater reassurance that the appropriate internal pressure has been achieved to restrain the product in the pouch. Product sensitivity can play a role in how much volume should be drawn out of the pouch.
- Reducing O2 or relative humidity (RH). Multiple vacuum/flush cycles can be programmed to progressively reduce the O2 or RH in the pouch. While modifying the atmosphere in the pouch can be programmed as a time-based function, vacuum and flush levels are critical in adequately and repeatedly reducing oxygen or relative humidity. That is why most applications requiring reduced O2 or RH operate in level mode. The flexibility of the pouch materials and their ability to conform around the geometry of the nozzle can affect the achievable goal, even with multiple cycles.
A chamber sealer is most commonly used for:
- Achieving ultra-low residual O2 Vacuum and gas flush applications requiring an extremely low residual oxygen level (below 1%) require a chamber sealer. A nozzle sealer cannot be used for these applications because of the “leak points” around the nozzle while it is processing the pouch. For ultra-low residual O2 level applications, the entire chamber atmosphere is modified and level setpoints as low as 1mbar can be programmed. A dwell time at each step can be programmed to maintain the level for the specified amount of time and allow the product to acclimate.
- Sealed header pouches. Sealed header pouches that need to be vacuumed and/or flushed must use a chamber sealer because it is physically impossible to insert a nozzle into a hermetically sealed and terminally sterilized pouch. In these cases, the atmosphere inside the pouch is modified by vacuuming and/or flushing through the Tyvek window on the pouch. For this type of application, a program that has the flexibility to allow multiple steps in either direction (vac-vac-vac-flush-vac-flush-flush, for example) with programmable dwell times at each step will provide the control required to vacuum the pouch without bursting it or to flush the pouch without crushing the product or pinching off the header. The atmosphere inside the chamber can change significantly faster than the interior of the pouch because the header acts as a filter, hampering the flow of air and/or gas into and out of the pouch. A dwell time at each vacuum or flush step can provide the necessary time for the pouch to acclimate to the chamber atmosphere before the next process step begins.
Pouch materials impact whether a nozzle or chamber should be used for applying a vacuum or a vacuum and gas flush
The pouches used for vacuum (no gas flush) and vacuum and gas flush applications are typically made from laminated or mono-layer flexible materials including—but not limited to—Tyvek, coated foil, and film. The specific materials used impact whether a nozzle or chamber is optimal, and these are the most common pouch material combinations and the method that works best for applying a vacuum and/or gas flush to each one:
- Foil/Foil: Nozzle or chamber
- Film/Foil: Nozzle or chamber
- Film/Film: Nozzle or chamber
- Foil/Tyvek Header: Chamber
- Film/Tyvek Header: Chamber
- Film/Tyvek: Nozzle
Other factors to consider before deciding to use a nozzle to apply a vacuum or a vacuum and gas flush to a pouch
A number of different factors should be considered before deciding to use a nozzle sealer to apply a vacuum or a vacuum and gas flush to a pouch. Here is a sampling of the top concerns:
- Headspace. Since using a nozzle involves employing a clamp between the guarding and the sealing die, the pouch must have sufficient “free” material (i.e., headspace) for loading into the sealer.
- Nozzle length. In order to be able to load the pouch over the nozzle, the nozzle must extend out of the sealer at least ½” resulting in nozzle penetration into the pouch of typically at least 1½” for constant heat sealers.
- Product sensitivities. If the nozzle must not come into contact with the product, the pouch length must be sized appropriately to allow the product to remain safely distant from the nozzle.
Other factors to consider before deciding to use a chamber to apply a vacuum or a vacuum and gas flush to a pouch
Before deciding to use a chamber to apply a vacuum or a vacuum and gas flush to a pouch, it is important to consider factors such as:
- Immobilizing the pouch. It is critical to immobilize the pouch during the vacuum and flush process. The air inside the chamber can become turbulent, and if the pouch shifts out of alignment with the seal bar, the pouch will not be sealed correctly.
- Cycle time. The cycle time when using a chamber sealer will always be longer than when using a nozzle sealer because of the volume of air that is being modified. A nozzle sealer is modifying only the interior of the pouch. By contrast, a chamber sealer is modifying the volume of the entire chamber and the pouch. Additionally, processing a header pouch for a low residual oxygen level application requires the most time and may require multiple vacuum/flush steps with dwell times at each step.
- Window for visibility. Using a chamber sealer that has a window for viewing the pouch as it is being processed can have enormous benefits. A window allows visibility into the process and enables the operator to monitor how the pouch is behaving during the vacuum, flush, sealing and repressurizing process.
The process for using a nozzle sealer to apply a vacuum or a vacuum and gas flush to a pouch
Using a nozzle sealer to apply a vacuum or a vacuum and gas flush to a pouch is a relatively straightforward process involving eight distinct steps:
- Bring the nozzle into the load position
The nozzle used to apply a vacuum or a vacuum and gas flush to a pouch is like a snorkel or “straw.” In the first step of this process, the operator presses a foot switch that brings the nozzle into the load position. - Load the pouch over the nozzle and slide it into the seal area
With the nozzle in the load position, the operator places the pouch over the nozzle and slides it into the seal area. - Close off the pouch around the nozzle
Next, the operator presses the foot switch a second time, bringing a soft-faced clamp down to close off the pouch around the nozzle. - Initiate the vacuum process, followed by gas flush, if needed
Once the pouch is closed off around the nozzle, the vacuum process can begin. If a gas flush process is programmed, the gas will flush the pouch upon completion of the first vacuum process. Additional vacuum and gas flush cycles can be programmed depending on the application requirements. - Apply final cycle
The cycle can be programmed to end after a flush step, leaving a “pillow effect” in the pouch, or it can be programmed to end after a vacuum step, drawing the pouch down around the product. - Retract nozzle while clamp is still engaged
Once the vacuum/flush cycle has fully completed, the nozzle retracts from the pouch while the clamp is still engaged. - Actuate seal bar and seal the pouch
After the nozzle is clear of the seal area, the seal bar actuates and seals the pouch. - Releasing the pouch from the sealer
In the last step of the process, the seal bar and the clamp open, releasing the pouch from the sealer.
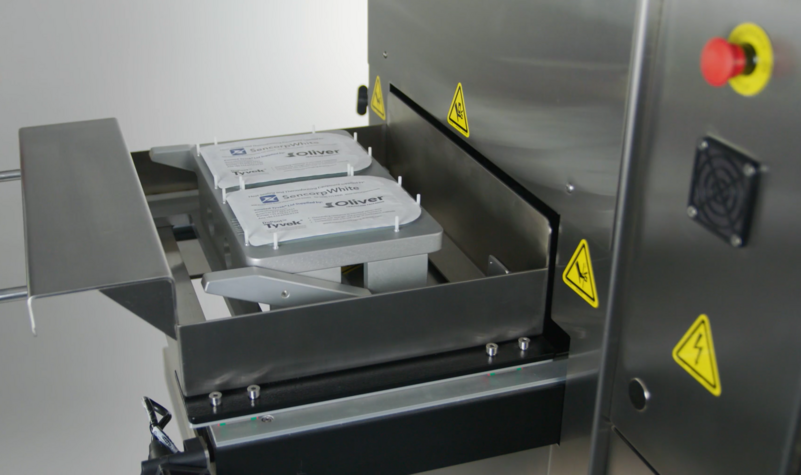
The process for using a chamber sealer to apply a vacuum or a vacuum and gas flush to a pouch
Using a chamber sealer to apply a vacuum or a vacuum and gas flush to a pouch is a relatively straightforward process involving eight distinct steps:
- Load the pouch onto a platform in the chamber
When a chamber sealer is used to apply a vacuum or a vacuum and gas flush to a pouch, the process begins when the operator loads the pouch onto a platform inside the chamber sealer. - Close the lid and apply the vacuum
Next, the operator closes the lid of the chamber sealer and initiates application of the vacuum. The entire volume inside the chamber is vacuumed until the programmed level is reached. - Initiate the gas flush
The gas flush process begins after the initial vacuum step(s) are completed and flushes the entire chamber to the programmed setpoint. - Apply additional vacuum and gas flush cycles as needed
Additional vacuum and gas flush steps can be programmed to achieve even lower residual oxygen levels. - Shuttle the pouch into the seal area and apply the seal
Once the vacuum/gas flush process is completed, the pouch is shuttled into the seal area and the seal bars close, sealing the pouch. - Shuttle the pouch back to the load position
After the seal dwell timer has elapsed, the pouch is shuttled back out into the load position. - Repressurize the chamber and open the lid
Next, the chamber repressurizes back to atmosphere and the lid opens. - Remove the pouch from the chamber
Finally, the operator removes the pouch from the chamber.
This blog post covered several of the primary issues you need to consider when determining how best to apply a vacuum or a vacuum and gas flush to pouch. For more information and to discuss the details of your particular application, please contact us.